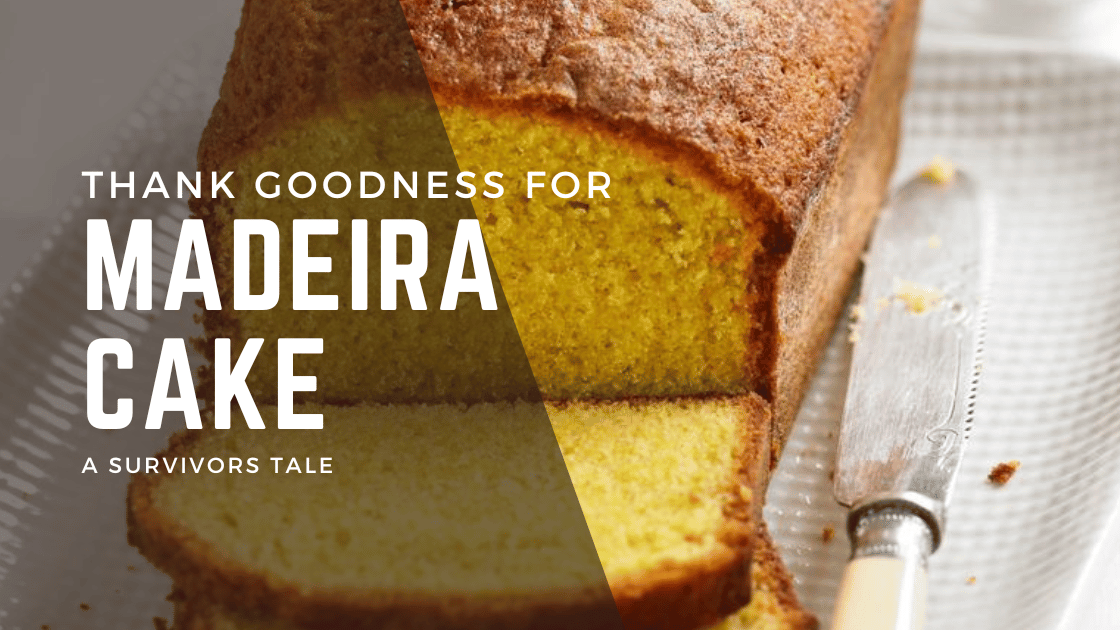
Thank goodness for Madeira cake!
Friday, April 5th, 2019, began like any other. I was 61. My wife has had MS for 38 years and is wheelchair-bound, and I work from home. Friday is the day our cleaner comes, and I often bake something, as much for therapeutic reasons as anything else. That day, I decided to bake a Madeira … Read more