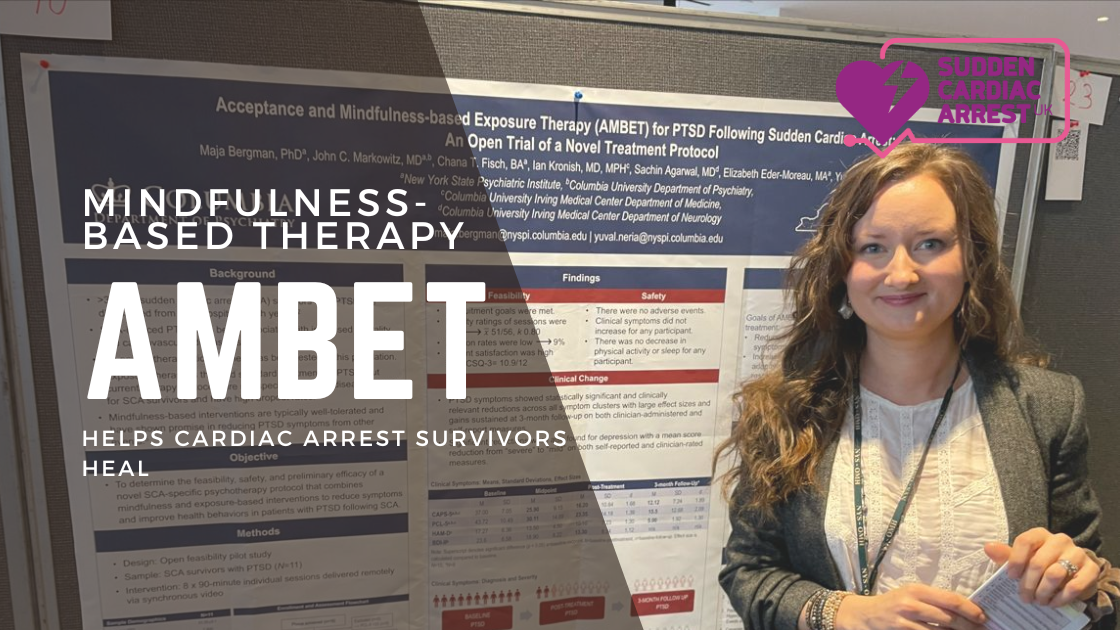
A Ray of Hope: Mindfulness-Based Therapy Helps Cardiac Arrest Survivors Heal
Surviving a sudden cardiac arrest (SCA) is an incredibly traumatic experience. While the initial relief of being alive is undeniable, the aftermath can be a harrowing journey. For many SCA survivors, the road to recovery is paved with mental and emotional turmoil, often leading to the development of post-traumatic stress disorder (PTSD). This debilitating condition … Read more